Low back pain is common and can have a detrimental impact on the ability to continue to work and your favourite activities. Despite the large impact on life, most cases of low back pain are not serious and do not require medical intervention. Even persistent and disabling chronic low back pain is not synonymous with significant tissue damage and pathology. It may seem counterintuitive, but severity of pain does not directly correlate to the severity of injury.
Recent MRI studies have shown that disc bulges, degeneration, osteophytes and other scary sounding findings are actually very common and many people have these findings on imaging but have no pain at all. In fact many of these changes may occur naturally as we age. Furthermore, we know that unnecessary x-ray and MRI among people with low back pain can lead to fear avoidance behaviours and negative coping strategies that can delay their recovery at best, and lead to poorer outcomes at worst.
Although unlikely to be serious, the specific cause of your low back pain may be complex with many factors contributing to your pain. It’s not all about injured tissues. Contrary to common belief, the degree and type of tissue injury is just one factor among many that will directly influence your pain. Moreover, if your pain has lasted longer than 3 months, factors other than tissue damage are more likely to be contributing to your pain. This is because tissue (i.e. nerve, muscle, joint, disc) healing occurs within the first few weeks to months.
Low back pain is best seen as a protective mechanism in response to your body’s perceived level of danger, threat or disruption to maintaining a balance within your body systems. Many contributing factors can have a beneficial or negative impact on the presence of your pain. This multi-factorial blend of physical factors (load management, tissue injury), psychological factors (ways of thinking about your injury, fear avoidance behaviours), social factors (stress, job demand flexibility, and home environment), lifestyle factors, among others can be involved and should be considered in treatment of your low back pain.
So what does this mean? Even in cases of severe pain, your low back pain is unlikely to need medical or surgical intervention. Treatment of your low back pain should include consideration of all potential factors contributing to your pain - not just the tissue that you have injured. Also, you are unlikely to need imaging to identify the source of your pain. In fact, this may work against you if you are responding well to physiotherapy care.
We know that a positive mindset is associated with lower levels of pain and disability. Once serious red flags are ruled out, a focus on movement within tolerable levels, graduated return to activity and exercise is recommended. Knowing the facts better prepares you to progress towards recovery. Check out these top 10 facts below:
Adapted from O’Sullivan, Caneiro, O’Sullivan, Lin, Bunzli, Wernli & O’Keefe. (2020). Back to basics: 10 facts every person should know about back pain. British Journal of Sports Medicine, 54(10), 698-699. DOI: 10.1136/bjsports-2019-101611
No referral is required to receive physiotherapy care. A clinical assessment by one of our physiotherapists will first rule out any red flags indicating serious pathology (with imaging only if necessary) followed by a physical assessment and a tailored treatment plan.
Your physiotherapist will work with you offering manual therapy to manage pain, expertise in load management and exercise prescription, assist you in developing positive coping strategies, identification of your specific contributing factors to your pain and assistance with a graduated return to doing the things you love. If required, other healthcare practitioners may be included in your treatment such as sports doctors, pain specialists or surgeons. You can expect expert advice and treatment allowing you to feel better, sooner.
Want to get started right now? General advice for people suffering from low back pain includes keeping active within tolerable limits, avoiding bed rest, using non-steroidal pain medication if required and continuing to work if possible (with job modifications if necessary).
Not sure if physiotherapy can help you? Book a complimentary 15-minute telephone consultation to discuss your specific case with a physiotherapist and receive advice on your next best move.
Are you eligible for the Careway Pathway? Careway is an escalated care pathway that ACC fully funds. If eligible, an individualized treatment plan will be devised on entry by a physiotherapist to assist you in achieving your goals. Following this, you will be connected with a team of healthcare professionals ensuring faster, coordinated care in diagnosis and delivery of treatment, facilitating a faster recovery. Your healthcare team may include sports physicians, physiotherapists, orthopaedic surgeons, vocational therapists, and pain management specialists. With no out-of-pocket costs and a connected team of health professionals, you will get the treatment you need -when you need it. Allowing you to get better, faster.
Learn more about how physiotherapy can help you with your low back pain and determine if you are eligible for the Careway pathway. Call us or book your appointment online today.
Traditionally, yoga is a physical and mental practice that originated in India. However, despite its ancient origins, yoga has continued to develop over time and is suited to everyone.
Yoga is a mind and body practice. It combines physical postures, breathing techniques, and meditation/relaxation. A regular yoga practice promotes strength, flexibility and calmness, which supports a well-balanced, active lifestyle.
During class, your teacher will guide you through various postures and breathwork. You can expect a warm-up with basic postures and breathing exercises. The class will then flow into a combination of movements and poses to challenge you physically. To cool down, more stretches and breath work will be incorporated.
It is a great form of progressive exercise for rehabilitation purposes after injury or for those who struggle with chronic pain. Whether you are recovering from injury, surgery, chronic back pain or looking to improve your general well-being, yoga can be of benefit.
For those deskbound at work, go ahead and try these! Performing these types of yoga stretches periodically throughout the day will help combat postural imbalances associated with desk-based work and stress.
It’s important to find a knowledgeable teacher who will guide you through your yoga journey safely and efficiently. Our yoga teacher at Auckland Physiotherapy, Mira, is both a physiotherapist and movement practitioner, having completed her yoga training back in 2018.
We look forward to seeing new faces join our studio for physiotherapy-based yoga classes, which include duet and private classes depending on your needs. We'll be starting these classes in July, so register your interest below and we'll let you know as soon as you can book in.
Most people who are unfamiliar with the Pilates method may think that the main benefits are simply improvements in posture and flexibility, but it goes far beyond that!
Whether you are looking to rehabilitate an injury, improve overall strength and mobility, or enhance athletic/sports performance, Pilates is an excellent exercise method to add to your lifestyle.
Pilates is low-impact, yet highly effective for enhancing your mind-body connection, regardless of your fitness level. There is a strong emphasis on sufficient breathing and working the body as an integrated whole, which massively improves your coordination and musculoskeletal function. Ultimately, this prevents the risk of injury and thus promotes a better quality of life.
Wanting to feel less ‘stiff’ in the joints and more supple and mobile? Pilates engages your body through different planes of movement in a controlled and repetitive manner. This stretches and strengthens the deep muscles surrounding your joints, so that you are able to move your joints comfortably and confidently through a range of motion that they were designed for.
Your core not only comprises the abdominal muscles, but also the diaphragm, deep postural muscles in the spine and pelvic floor. Challenging your core with a variety of movement patterns, along with the correct breathing technique, can help strengthen and stabilise your core and translate to everyday activity and/or athletic performance.
I’ve only named a few of the myriad benefits Pilates has on your overall well-being. So, the next best thing you can do now is to give it a go (with consistency and effort, of course) and experience the positive changes for yourself! Contact Auckland Physiotherapy to help you begin your journey into the world of Pilates.
Well… How are you feeling?
Whether you are currently pregnant, or you are in the process of recovering from childbirth, surely you are appreciating just how much your body can transform to meet the demands of growing a baby. This can shake the confidence of even the most body-aware women. What activities are safe? What is beneficial? What is just normal pregnancy discomfort and what can be eased with some clinical management?
The childbearing years are a journey through a period of what can feel like constant change for our bodies.
The pre and postnatal WOFs are designed for those who are really after information and feedback in a one-off session (though the WOF can lead on to further management if this is indicated). If there are specific concerns or questions, these will be addressed, and if further clinical management is indicated this can flow on in consecutive sessions.
The WOF session is really guided by what you need; what are your concerns, how are you going with exercise, what is your history with exercise, do you have any history of incontinence or perineal problems, and what are your goals? Though there is plenty to go through even if you don’t have a complete list of questions!
What you can expect from your pregnancy WOF:
What you can expect from your postnatal WOF:
NB: if you have had any perineal pain or trauma, it is more likely that you will need a postnatal women's health appointment, and possibly some follow up, where we will focus more on the perineum recovery and any concerns related to this.
We have loads of information on our women's health section of our website, including conditions specific to women's and pelvic health that we manage daily in our clinic, as well as an online shop for many products related to pregnancy, postpartum, and pelvic health.
Someone once asked me, is the point of meditation to clear your mind and think of nothing?
The brain is like the heart... the heart continually beats, just like the brain continually thinks. We have 60,000-80,000 thoughts a day! It is pretty impossible to stop thoughts from coming during meditation. So please don't think this is the ultimate goal!
The point of mindfulness meditation is to give your brain a new task and to simply observe your thoughts without judgement, bodily sensations, and breathing, and learn to control how you are reacting to these thoughts, feelings and sensations. This can then result in feeling calmer, an increased sense of acceptance and letting go through forgiveness, and it can improve resilience, gratitude, and patience in daily life.
The first challenge of meditation is to be able to sit with yourself in stillness, with your thoughts and tuning into your body and breath.
SO... is mindfulness & meditation practise for everyone? In extreme and acute mental health situations, one should be cautious as it can turn up the volume of your thoughts and awareness. But otherwise, in most cases, it is a very beneficial tool to help improve mental well being. Research has shown that mindfulness practice and meditation are effective and holistic methods to reduce stress, ease the anxious mind, improve discipline and emotional intelligence and resilience, improve sleep and develop a happier, more positive perspective on life.
My bespoke 4-week Mindfulness-Based Stress Reduction (MBSR) course is carefully designed to teach you the principles and practice of mindfulness, for the lifestyle challenges we can face day-to-day. Individual, smaller group or corporate sessions are also an option should you wish to do this.
Learn to find the balance between 'doing and being modes', and that calm clarity between your thoughts and reactions.
Contact Renée for a free phone consultation regarding her Mindfulness courses and individual sessions, and to also ensure eligibility to join. Email Renee at [email protected] or book HERE for a complimentary phone call.
We are almost a quarter of the way through 2022, a year where we all started off with more hope that this year would be different and we’d get back to living life the way we did before. But so far that hasn’t been the case and for many people, it might feel like the hangover of last year’s lockdown hasn’t subsided...
If you’re feeling unmotivated, out of sorts and generally still a bit (or a lot) stressed then know that you aren’t alone. The ongoing effects of this pandemic are still bubbling away. From talking with many of the team here at AP it’s a trend we’re definitely seeing more of in the clinic - our clients are reporting more niggling and nagging injuries that are taking longer to settle, ongoing stress and anxiety, poor sleep patterns, altered work, home life and exercise regimes and an overall difficulty getting back into any sort of routine as everything around us continues in a state of flux.
As a health coach, a huge part of my job is to help people change their behaviour to support and optimise their health, particularly through times of adversity. I know that our team here at AP has an armoury of tools that we teach people time and time again. Very often, we see them pick up those tools, make some changes and go away feeling better. But does it last? Just because we told you to do it, will the change stick? What makes you carry on with those health-enhancing behaviours once your appointments stop? Very often, life gets busy and good intentions fall by the wayside. And given that we’re all humans here too, we know that the wayside is usually mere seconds away!
So how do you prioritise your physical and emotional wellbeing? How do you choose strategies and coping tools that not only work for you but are ones that you’ll keep practising even when times are tough?
If you’re still reading this blog, chances are you’ve already started to consider looking after your wellbeing. And somewhere in that thought process, you may have begun to consider why it’s important to you. So, let's have a go at making that a little more formal.
What would your answer to this question be?
“Why is it important for me to look after my physical and emotional health?”
Your first answer will give you some information but is likely to be a bit on the superficial side. So let's ask ‘why’ again and keep going until we start to hit the real heart of the matter. It might look something like this:
Answer one: because I’ve been feeling really stressed
Why is it important to you to feel less stressed?
Answer two: because I become a really grumpy person when I’m stressed
Why is it important not to be so grumpy?
Answer three: because I often feel guilty at the end of the day for being that way with my family
Why is it important to you to change how you feel at the end of the day?
Answer four: because I’m so busy and I feel like I have so little time with my family that I want it to be happier. Life seems to move so fast and I don’t want to miss out on the time we do have together.
Why is that important?
Answer five: because I want them to feel loved and connected to me
Asking why (as many times as you need to, there’s no magic number) can start to give you a sense of what’s driving you to consider your wellbeing. You can see in this example that talking about the desire to decrease an unpleasant feeling, in this case stress, moved to unearth a couple of fairly powerful values: love and connection. This exercise requires you to slow down and consciously consider the deeper drivers that underpin your motivation in any given instance.
This simple exercise of asking ‘why’, applied to all sorts of situations, can really start to help you gain a little clarity. You may not come up with all the answers right away and that’s perfectly ok. Think of this as an experiment; you’re constantly collecting data and learning more about what’s worth keeping and what’s worth chucking. Along the way, you’ll begin to uncover a clearer sense of who you want to be, and that’s pretty crucial if you want to be effective in making change.
So, you’re beginning to understand your ‘why’ - but what helps you steer the course?
They are, at the simplest level, the things you find meaning in life. They’re what you care about and consider to be important. For example, ‘kindness’, ‘connection’ and ‘achievement’ are all values, as are ‘health’, ‘community’ and ‘challenge’. When we have clarity over our values, we can use them as a filter for our decisions and as a guide to our actions. This helps us to make more ‘towards moves’ in line with what we really care about, rather than being dragged along by life in a series of ‘away moves’ which leaves us feeling unhappy, unmotivated and unfulfilled.
So how do you know which values are important to you? There are many different exercises to help uncover the answers to this but let’s have a crack at this visualisation exercise…
Close your eyes and imagine you’re sitting in a nice room or a beautiful garden, somewhere you feel comfortable. Take a moment to acknowledge the body you are in and the mind that comes with you. This body, this mind, has been with you for many years, working hard to make a happy life.
Now imagine you’re in your later years, sitting in the same spot contemplating the life you’ve lived. As you look back, you feel a deep sense of satisfaction, joy and contentment. Life hasn’t always been easy but you’ve managed to stay true to yourself to the best of your ability.
Which core values are represented in this life?
What values came through for you? Generosity? Knowledge? Creativity? Health? The list can be long and if you’re just beginning this journey maybe talking about values with people you trust could help further define them.
Now here’s where you often start to have more questions than answers. A few common ones might be:
Are any values more important than others? Nope!
Should my values always stay the same? Nope!
Can I have more than one value? Sure!
Life changes and so it makes sense that your values change as you go through different stages. What matters here is that you have some sense of what’s important to you. The impetus to keep going when the going gets tough…
So you’ve defined your ‘why’ and your underpinning values. This has helped to hone in on what’s important to you, identify what to prioritise and where to put your precious time and energy. Having a clear sense of your values ultimately enhances your motivation, making it more likely you’ll stick with your plan of change. But what about actually doing it? How do you ensure that when (not if) your initial plan starts to waiver, you can stick with it?
In his book ‘Atomic Habits’ James Clear defines three levels of behaviour at which change can occur:
Outcome - what you get
Processes - what you do
Identity - what you believe
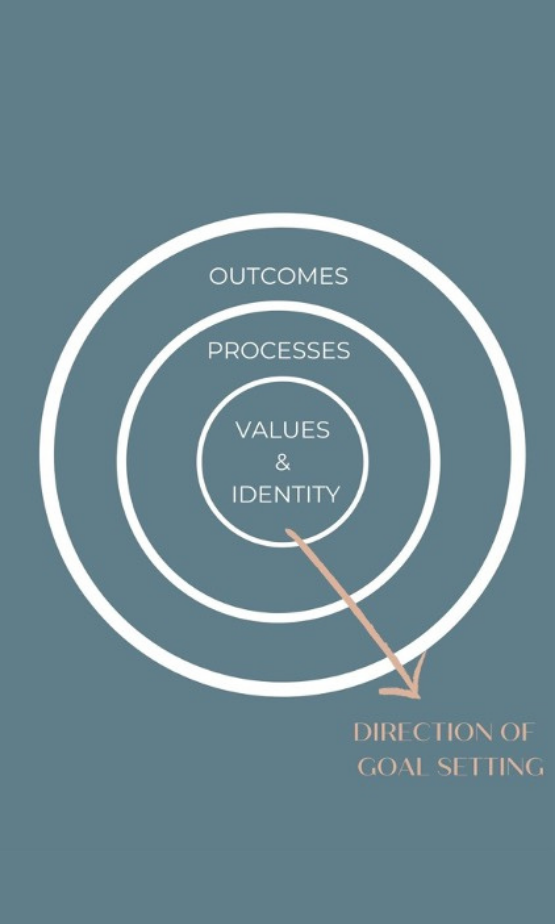
Most of us will be familiar with setting a goal based on the outcome we want, like being able to run 5km, earning more money or losing weight. So then we decide on a process to achieve that goal and go about implementing it. More often than not, life gets busy, we have setbacks and it gets hard to maintain that process so we fall off the wagon.
How about if we flipped the way we set our goals? This is called identity or values-based goal setting. We start with ‘our why’ or our values and create a process that reflects that, and whilst we care about the outcome, it’s not the main driver for our behaviour or actions.
We hone our focus on the process. Here it's all about small wins. Changing habits is a tricky business and your brain can be pretty hard-wired to work a certain way. If you’re trying to change things up, the kindest way to do this is through a series of small wins. Translated, that means MAKE IT EASY, so easy that you almost can’t fail. I think we can all relate to the idea that we need success to help us move forward, repeatedly setting ourselves an unsustainable target isn’t worth anyone’s time and energy.
So you’ve figured out your ‘why’, you're becoming clearer on your values and you have some small actions you can take to achieve that values-based goal. Hopefully, if you’ve made the actions small enough then chances are you’re already feeling pretty confident to get going with that today. And if you keep applying this formula you’re well placed to implement some really great tools to look after yourself and re-create some routine in your life.
Still feeling a little lost? Maybe you want to delve into what this looks like specifically for you? No problem! Book in for a complimentary 30-minute Health Coaching call to give you a taste of what Health Coaching could do for you. Or if you’re already sure that Health Coaching would be of benefit to you, you can book online to get started straight away with one of our package deals.
Compiled by our Director, Senior Physiotherapist and Pilates Instructor Helen Dudley. To book an appointment with Helen, or read her Meet the Team profile CLICK HERE.
Incontinence is the involuntary loss of urine at an inappropriate time or place. For a lot of us, incontinence can be an everyday occurrence that puts strain on our mental health and can limit our physical activities and enjoyment. This taboo problem is unfortunately all too common so if you do experience incontinence, whether it is a few drops every now and then to full bladder leakage, you’re not alone. In fact;
- 1 in 3 women have some degree of urinary incontinence
- In women 45-60 years old, this number increases to 50%
- 13% of men have urinary incontinence
As Physios, we obviously advocate the assessment and rehabilitation of incontinence issues with a Pelvic Health Physiotherapist, especially as the research is so propelling as to the success of treatment. In fact, 70% of women with incontinence will get significant improvements with appropriate treatment.
In saying that, we also understand that it can be very debilitating to every day life so management is just as important to enable you to live well and do the things you love. In the past, this has meant using pads that are uncomfortable and not environmentally sound. That is why we were so excited and had to share this great new product with you.
Awwa is a great NZ female founded company that provides pee-proof pants for people of all shapes and sizes. They have a great ethos; making sustainable and climate positive products that are made of natural, organic and recycled fabrics. The pee-proof underwear wicks moisture away from the body and locks it into the centre layer, meaning you feel dry and smell fresh all day long.
Here is more information taken from their website:
How Does AWWA work for bladder leakage?
Our innovative hi tech layers have been developed especially to absord fluid but keep you dry and fresh.
1 - The top layer, sits closest to your skin and wicks moisture away fast and keeps you feeling dry.
2 - An antimicrobial layer that fights odours and bacteria
3 - A super absorbent layer that safely holds 18 ml of fluid (that you do NOT feel)
4 - Bottom layer, is a leak proof barrier
Do they smell?
Our high tech layers mean that all liquid and odour are locked in the middle layer so there’s no smell.
Do you feel wet wearing them?
Absolutely not!
How long can you wear incontinence underwear before changing them?
This comes down to what you’re comfortable with, but our underwear can hold up to 18ml so you should be able to wear one pair all day long.
They are great for periods too. Our absorbent technology supports you through pregnancy and incontinence. Making us period proof, postpartum proof and pee proof with a range of absorbency levels and styles to suit you.
What AWWA styles do you recommend for incontinence?
We recommend the Eva brief, Cotton Brief or Skye High styles
AP have created a health solution company called The Health Collective. The collective consists of a group of trusted experts in the health and wellness field that have personally selected products that will assist our communities health and wellness.
We stock a wide range of select locally produced, ethically sourced, sustainable products to help you keep healthy, recover from injury, support you while you work and play, help you to sleep and relax and to support women during pregnancy, postpartum and beyond.
Compiled by our Masters trained Physiotherapist Chris Smith. To book an appointment with Chris, or read his Meet the Team profile CLICK HERE.
Foam rollers have grown in popularity over the last decade as a key piece of kit in gyms and home exercise settings. Their uses may vary from warm up prior to exercise, to for recovery afterwards, or simply to increase flexibility to aid in an exercise program. But what benefits do foam rollers provide us with and how might these be achieved in practice?
Research
A recent research review looking at the efficacy of foam rollers found they were better for some things that others (see here). For example, there may be a benefit in sprint performance following pre-foam rolling prior to sports activity. However, in recreational athletes, up to 62% of the population are likely to experience benefits in flexibility from pre-foam rolling as a warm-up prior to sport. Furthermore, this increased flexibility has been shown to be produced from as little as 30 seconds on a foam roller in the hamstring muscles. It has been suggested that these benefits may be due to increase in intramuscular temperature and blood flow. Also, foam rolling may stimulate pressure cells in our muscles which relay information to our brain to reduce pain sensation. This in turn may increase our stretch response to enable us to get a little more range in our downward dog!
When it comes to recovery, the main finding was that post-exercise foam rolling can help with reducing muscle pain sensation or soreness. This is important as muscle soreness has the potential to reduce performance in relation to sprinting, jumping and strength training. Therefore, if we can reduce soreness through foam rolling then this may provide some benefit to further athletic performance. However, this should not be used as an alternative to appropriate physical and mental rest, sleep and nutrition in your training to allow appropriate muscle and soft tissue recovery.
Application
Foam rollers can be likened to a form of self massage, providing some of the health benefits of manual therapy applied by a physiotherapist or massage therapist, although without that human connection and therapeutic relationship, which has a large role to play in positive outcomes. However, multiple lockdowns this year have left us working from home without the option of visiting our favorite therapists.Therefore, a foam roller provides a great self-management option during lockdown, holidays or when away on business and you can't see your therapist.
Take home message
A foam roller can be a great addition to your warm up routine. Only spend 30-60 seconds on each area and then perform a dynamic warm up and stretch routine after to increase flexibility and blood flow prior to exercise. There is no need to spend 10 minutes rolling an area. If you’re going to roll for recovery 2 x 45-60 seconds on each major muscle group to reduce muscle soreness as part of a cool down, which should include adequate physical and mental rest, sleep and nutrition.
If you don't yet have a foam roller as part of your exercise equipment visit our online store to see our range on offer.
Compiled by our Masters trained Physiotherapist Kirsten Rose. To book an appointment with Kirsten, or read her Meet the Team profile CLICK HERE.
What is a Health Coach?
Most people want to be healthy and well, but there is an enormous gap between those thoughts and the everyday reality of actually making it happen. Nearly all of us can probably identify with a time in our lives where we wanted to get healthier, be more active, lose weight, be less stressed, be happier….the list can be endless. Also most of us can probably reflect on how making the required changes was much harder than we might have initially thought it would be. We start off with a hiss and a roar, but then our motivation wanes, our old habits creep back in, and we give up on our new way of life. Sound familiar?
If your answer is yes, then don’t beat yourself up too much. Inside every one of us is the urge to stay with the status quo, resisting change or challenges outside of our comfort zone. There’s another part, deep inside, that whispers to us that maybe we could change, maybe we could actually achieve those health goals and live the healthy lifestyle we dream of. But change is hard so those whispers often don’t get the chance to grow louder. The reality is that most of us need to build new life skills in order to create a truly sustainable plan for our well-being. We need to learn to believe in our own ability to take charge of our health and to implement the necessary changes. Our day-to-day lives are full of small choices that could help us inch our way to the life we want to create, however, in the modern day world there appears to be an overwhelming amount of choice so often we don’t know which ones are right for us.
Health Coaching encompasses the sciences of positive psychology, behaviour change, nutrition, exercise science and lifestyle medicine with the dynamic art of relationships, teamwork and community. As a Health Coach, I am a behavior change specialist who supports you to make sustainable diet, lifestyle, and habit changes that will actually work for you. I help you optimise your health and well-being by enhancing your resourcefulness, self-regulation, and self-motivation, so that you can successfully navigate the journey of change.
Some common areas that clients wish to work on include:
If you think that Health Coaching could help you on your journey to better health and wellness then take advantage of the 30 minute free sample consultation. These are available in the clinic or online.
Compiled by our Masters trained Physiotherapist Kirsten Rose. To book an appointment with Kirsten, or read her Meet the Team profile CLICK HERE.
Stress - Part 2
Where are you on the stress curve?
The Yerkes-Dodson concept is a model of the relationship between stress and performance. It’s a theory that has been around since the early 1900’s.
It shows us that stress can be seen as a continuum. Too little stress or challenge and we’re likely to become unmotivated. At this level, there’s often little incentive to perform well so we go about our routine but boredom sets in.
As the challenge increases, so does our motivation. A moderate amount of stress goes a long way in boosting our performance. We’re alert, thinking clearly and our brain and body are fired up to get the job done. This is called eustress. But this only works up to an ‘optimal point’.
After this point there’s too much pressure. Stress and anxiety ramp up and we are unable to perform to our full potential, despite the fact we may still actually want to perform well. Our stress response is now working against us and we are negatively affected both mentally and physically.
The Yerkes-Dodson law is particularly relevant during the COVID-19 pandemic. At times we may not be challenged enough - restricted social activities, boredom or lack of routine can easily rob us of motivation. Or at the other end, we may be feeling overly stress and anxious about work, family, finances and the general uncertainty. The combination of these can easily push us down the other side of the curve.
Where do you think you are sitting right now? Auckland Physiotherapy Director and Masters Physiotherapist, Mark Quinn, shares his experience with stress. If you read the previous blog about the different components of stress, can you pick these out from Mark’s description? (Thoughts, feelings, behaviours, physical reactions). What could you do to move yourself back into the optimal zone?
Mark, when does stress make you perform better?
Stress makes me perform better when I manage to keep my discipline while managing my workload, family life, and ensuring I continue to work on the things that help to mitigate the negative effects. I do love a good challenge and getting through a list of jobs but if this becomes too much it can lead to overwhelm so I am learning how to manage that.
'Healthy stress' gets me up in the morning (not too early), encourages me to do all my jobs that I need to before I start the day and at the end of the day leaves me feeling satisfied with enough in the tank to have fun with my son and partner in the evenings.
How do you know when your stress is becoming too much/negatively impacting you?
I start to wake up in the middle of the night and have difficulty getting back to sleep. Anxiety creeps in. I also start to work too much and drop off my exercise and meditation which I know really helps me. My partner would probably say that I become less positive (a nice way of saying I get grumpy).
What's your go to for managing stress for yourself?
I have to work hard on limiting my work hours (I tend to over do it) so have a reminder on my phone - no screen time from 7pm onwards... this basically means get off your phone and stop doing work but I do allow myself to watch tv as this helps me to wind down. Exercise, meditation, and ensuring I have some down-time that is not screen time. For me that is getting out in nature, going for a swim, or hanging out with friends and family.