Physiotherapists are highly trained healthcare professionals who specialise in the assessment, treatment, and prevention of physical conditions that affect movement, function, and overall well-being. Many people associate physiotherapy with recovery after major injuries, but physiotherapists are equipped to treat a wide range of conditions, from acute injuries to chronic pain and even long-term rehabilitation after surgery.
Physiotherapists work closely with Gp's and Specialists. They can submit ACC forms and send you for X-rays, ultrasounds and some cortico-steriod injections.
Knowing when to see a physiotherapist can sometimes be challenging, especially when symptoms are mild or you’re unsure of the severity of your condition. In this blog, we’ll explore key signs that indicate it’s time to consult a physiotherapist and how early intervention can help improve your outcomes.
1. Persistent Pain That Doesn’t Go Away
One of the most common reasons people visit a physiotherapist is because they’re experiencing pain that persists longer than expected. If you’ve had pain for more than a few days and it doesn’t seem to improve with rest or over-the-counter medications, it’s a good idea to seek professional help. This is especially true if the pain starts to interfere with your daily activities.
Common scenarios:
Back pain that doesn’t resolve after a few days of rest.
Neck pain or stiffness that persists despite self-care measures.
Joint pain that affects mobility or gets worse with certain movements.
Physiotherapists can assess your pain, pinpoint the underlying cause, and provide treatments such as manual therapy, exercises, and advice on posture and ergonomics to reduce discomfort and speed up recovery.
2. Acute Strains and Sprains
Acute strains (injuries to muscles or tendons) and sprains (injuries to ligaments) are common injuries that often occur during physical activity or accidents. These injuries can be painful, limiting your ability to move the affected area. While rest and ice are essential in the initial stages, physiotherapy can help speed up recovery and reduce the risk of re-injury.
How physiotherapy helps with acute strains and sprains:
Pain management: Physiotherapists use techniques like ice therapy, ultrasound, or TENS (Transcutaneous Electrical Nerve Stimulation) to manage pain and inflammation.
Rehabilitation: Strengthening and stretching exercises to restore function and flexibility.
Preventing future injury: Educating patients on proper movement patterns, postural alignment, and strengthening exercises to reduce the risk of recurring injuries.
For sprains and strains, early physiotherapy intervention can reduce recovery time, improve healing outcomes, and help you return to your activities sooner.
3. Injuries that Don’t Heal Properly
Sometimes injuries don’t heal as expected, or they continue to cause issues months after the initial injury. If you've injured yourself and the healing process seems to be taking longer than anticipated, or if you're still experiencing functional limitations after an injury, a physiotherapist can help ensure proper recovery.
For example:
A sprained ankle that still causes swelling or difficulty walking after several weeks.
A shoulder injury that limits your range of motion or strength, preventing you from participating in normal activities.
A knee injury that doesn’t seem to get better despite at-home treatments.
Physiotherapists can assess whether the injury has healed correctly, check for muscle imbalances or stiffness, and provide targeted rehabilitation exercises to strengthen the area and prevent future injuries.
4. Post-Surgical Rehabilitation
After surgery, physiotherapy plays a crucial role in helping you recover and regain full function. Whether you’ve undergone a joint replacement, spinal surgery, or any other major procedure, physiotherapy can assist in the rehabilitation process to ensure a faster and more complete recovery.
Benefits of physiotherapy after surgery include:
Reducing scar tissue buildup.
Regaining strength and mobility in the affected area.
Preventing complications like joint stiffness or muscle atrophy.
Returning to your activities of daily living and sport
A physiotherapist will tailor a rehabilitation program based on your specific surgery and recovery goals. Early intervention can also reduce the risk of complications and promote a quicker return to everyday activities.
5. Chronic Pain Conditions
If you suffer from chronic pain conditions such as osteoarthritis, fibromyalgia, or sciatica, physiotherapy can offer significant relief. While medications may temporarily mask the pain, physiotherapists focus on addressing the underlying causes through exercise, education, and hands-on treatments to improve mobility and function.
Physiotherapists can help with:
Developing strengthening and stretching programs to reduce muscle tension.
Teaching proper body mechanics to reduce stress on joints.
Offering pain management techniques that can reduce the need for long-term medication.
For chronic conditions, early physiotherapy intervention can help reduce pain levels, improve quality of life, and slow the progression of the condition.
6. Rehabilitation for Postural Problems
Many people experience postural issues due to desk jobs, prolonged sitting, or improper ergonomics. Over time, poor posture can lead to back pain, neck stiffness, and headaches. If you’re noticing that your posture is causing discomfort or leading to more serious issues, a physiotherapist can help.
How physiotherapists assist with postural problems:
Assess posture and pinpoint areas of weakness or imbalance.
Provide exercises to strengthen key muscles that support good posture.
Advise on ergonomic adjustments in your workspace or daily activities.
Correcting posture not only alleviates pain but also helps prevent long-term issues like spinal degeneration or repetitive strain injuries.
7. Reduced Mobility or Difficulty with Movement
If you notice that your range of motion is decreasing or you’re having difficulty with activities like bending, reaching, or walking, physiotherapy can help restore function. Loss of mobility may occur after an injury, due to age-related changes, or as a result of medical conditions such as arthritis.
For example:
Difficulty bending your knee fully after a fall.
Limited ability to rotate your shoulder after surgery or injury.
Trouble walking or maintaining balance due to muscle weakness.
A physiotherapist will work with you to improve flexibility, strength, and coordination, as well as recommend assistive devices or techniques to help with movement.
8. Sports Injuries and Prevention
For athletes or active individuals, sports injuries are common. Whether you're experiencing a muscle strain, ligament sprain, or overuse injury, physiotherapy can play a key role in recovery and injury prevention.
Key benefits of seeing a physiotherapist for sports injuries include:
Diagnosis of the injury and development of a tailored treatment plan.
Rehabilitation exercises to restore strength and flexibility.
Advice on how to safely return to sport without the risk of reinjury.
Injury prevention strategies, including warm-up routines and muscle conditioning.
Early physiotherapy intervention can help reduce recovery time and improve performance, allowing you to get back to the sports or activities you love sooner.
9. Balance and Fall Risk Assessment
As we age, balance can become an issue, leading to an increased risk of falls. If you’ve experienced a fall or feel unsteady on your feet, a physiotherapist can assess your balance and help reduce the risk of future falls.
How physiotherapy can help:
Improving strength, flexibility, and coordination.
Teaching balance exercises to improve stability.
Recommending assistive devices, like canes or walkers, if necessary.
Physiotherapists can also develop a fall prevention program tailored to your needs, helping you stay independent and safe as you age.
9. Management of Headaches
Many individuals suffer from tension headaches, cervicogenic headaches (headaches originating from the neck), or migraines. Physiotherapy can offer a holistic approach to managing headaches, particularly those related to musculoskeletal issues. Poor posture, muscle tension, and neck stiffness are common causes of tension-type headaches, and physiotherapists are skilled in addressing these factors.
How physiotherapy helps manage headaches:
Manual therapy: Techniques such as joint mobilizations or soft tissue massage to relieve tension in the neck, shoulders, and upper back, which may contribute to headaches.
Postural correction: Improving posture to reduce muscle strain in the neck and upper back.
Stretching and strengthening: Targeted exercises to relieve muscle tension and strengthen weak areas that may contribute to headache pain.
If you experience frequent or chronic headaches, consulting a physiotherapist may help reduce the intensity and frequency of your headaches and improve your overall quality of life.
10. Acute Strains and Sprains
Acute strains (injuries to muscles or tendons) and sprains (injuries to ligaments) are common injuries that often occur during physical activity or accidents. These injuries can be painful, limiting your ability to move the affected area. While rest and ice are essential in the initial stages, physiotherapy can help speed up recovery and reduce the risk of re-injury.
How physiotherapy helps with acute strains and sprains:
Pain management: Physiotherapists use techniques like ice therapy, ultrasound, or TENS (Transcutaneous Electrical Nerve Stimulation) to manage pain and inflammation.
Rehabilitation: Strengthening and stretching exercises to restore function and flexibility.
Preventing future injury: Educating patients on proper movement patterns, postural alignment, and strengthening exercises to reduce the risk of recurring injuries.
For sprains and strains, early physiotherapy intervention can reduce recovery time, improve healing outcomes, and help you return to your activities sooner.
When to Seek Physiotherapy: Early Intervention is Key
While many individuals wait until their condition becomes severe before seeking physiotherapy, early intervention is crucial for achieving the best outcomes. If you notice any of the signs above, it’s a good idea to consult a physiotherapist sooner rather than later. Early treatment can help alleviate pain, restore function, and prevent the development of chronic issues.
Remember, physiotherapists are trained to treat a wide variety of conditions that affect movement, so don't hesitate to reach out for professional help. Whether you’re dealing with pain, recovering from an injury or surgery, or simply want to improve your mobility, physiotherapy can offer the guidance, treatment, and education you need to get back to your best.
Contact Us Today
If you’re experiencing any of the issues discussed above or simply want to learn more about how physiotherapy can help improve your quality of life, contact our our clinic (close to Remuera, Newmarket and Parnell) today to schedule a consultation or book in for a first appointment online. Our expert physiotherapists are ready to support your journey to better health and well-being.

Check out our Online Store for great Rehab and Health goods.


The Importance of Rest in Injury Recovery: A Vital Component in Physiotherapy
When it comes to injury recovery, the importance of rest often cannot be overstated. While many people associate recovery with active treatments such as exercise, physiotherapy, and rehabilitation, rest is an equally essential component. For physiotherapists, understanding the role of rest in recovery not only helps guide the treatment process but also ensures that patients can return to their activities stronger and with less risk of re-injury.
The Role of Rest in Healing
When a person sustains an injury, the body initiates a natural healing process that involves several stages: inflammation, repair, and remodeling. Rest is crucial during the early stages, particularly during inflammation and repair. During these phases, tissues are healing and repairing themselves, and giving them adequate rest helps to avoid unnecessary strain or stress that could impede this process.
1. Reduces Inflammation and Swelling
In the immediate aftermath of an injury, the body often experiences inflammation. Swelling, redness, and pain are common signs that the body is trying to protect the injured area and promote healing. Resting the injured area helps to reduce the physical stress on tissues, allowing the inflammatory process to proceed without exacerbation. Continued activity too soon can worsen inflammation and delay the healing process.
2. Promotes Tissue Repair
During the repair stage, cells known as fibroblasts play a critical role in building new tissue to replace damaged structures. However, for these cells to function optimally, they need time and energy to repair the damage. Resting the injured part of the body provides the necessary environment for these processes to occur without being hindered by additional stress or movement.
Active Rest vs. Complete Rest
While complete rest is often only needed for the first 1-3 days post an injury, active rest can also be beneficial during certain stages of recovery. Active rest refers to performing low-intensity activities that do not exacerbate the injury but help maintain overall mobility and circulation. This is where physiotherapists can play a pivotal role in guiding patients toward appropriate forms of active recovery, depending on the severity of the injury. They call it Optimal loading which actually helps to promote repair, remodel and build ligament, tendon and muscle tissue tolerance.
For example:
After an ankle sprain, a physiotherapist may recommend light stretching or range-of-motion exercises to maintain flexibility without causing further damage.
Following a muscle strain, walking or swimming at a gentle pace can promote circulation and reduce stiffness, aiding in the healing process.
Active rest encourages blood flow to the injured area, which supports the delivery of nutrients and oxygen essential for tissue repair. This approach helps prevent muscle atrophy, joint stiffness, and other complications of being sedentary for too long.
Preventing Re-Injury
Incorporating adequate rest into injury recovery is not just about allowing the tissues to heal—it also plays a key role in preventing re-injury. If a patient resumes activity too quickly without proper rest, there’s a high risk of reinjuring the same area, which can lead to a longer recovery time and potentially more severe damage.
Rest allows the body’s structures to regain their full strength before returning to normal activities. This is why physiotherapists often work with patients to gradually reintroduce physical activity through rehabilitation exercises designed to strengthen muscles, ligaments, and joints after an injury. Proper rest ensures that the body is fully prepared for these rehabilitative efforts.
Rest and the Mind-Body Connection
Physical rest is not only about giving the body a break, but it also helps improve mental recovery. Dealing with an injury can be mentally taxing, especially if the injury leads to prolonged inactivity or pain. Adequate rest promotes the mental clarity needed for patients to engage in rehabilitation activities effectively and without the mental fatigue that can accompany overexertion.
Additionally, when patients rest appropriately, they are more likely to stay motivated to complete their rehabilitation. An injury can be discouraging, but knowing that rest is a necessary and beneficial part of the healing process can help patients stay engaged and patient throughout their recovery journey.
Scientific Evidence Supporting Rest in Injury Recovery
Numerous studies support the idea that rest plays an integral role in injury recovery. For instance, research published in the Journal of Orthopaedic & Sports Physical Therapy has demonstrated that rest, especially in the early stages of injury, helps decrease inflammation and enhances the healing process. Other studies indicate that resting injured muscles reduces the likelihood of chronic pain or long-term damage.
One particular study highlighted in the American Journal of Sports Medicine showed that athletes who followed a rest period post-injury had significantly better recovery outcomes compared to those who resumed their activities prematurely. This finding emphasizes the importance of proper rest in minimizing the risk of reinjury and ensuring long-term recovery.
The Bottom Line: Rest is Essential for Optimal Recovery
As Physiotherapists at Auckland Physiotherapy, it is important to recognize that rest is not a sign of weakness or inactivity in injury recovery—it’s a critical component of the healing process. While it’s tempting to push through pain or resume activities prematurely, proper rest accelerates healing, prevents further damage, and ultimately leads to better outcomes.
A balanced approach that includes both rest and rehabilitation exercises is key. By guiding patients through the appropriate phases of recovery, physiotherapists can ensure that their patients return to their normal activities stronger, healthier, and with a reduced risk of future injury.
Remember, healing is a process that takes time, and respecting the need for rest is one of the most powerful tools in achieving long-term recovery.
For more information and help in your recovery, come into our clinic (close to Remuera, Newmarket and Parnell) to speak to our expert team. It is essential you first get the right diagnosis before any treatment and management occur so book in for a first appointment.

Check out our Online Store for great Rehab and Health goods.


Yes, physiotherapy can be very helpful for managing osteoarthritis (OA). While it cannot cure OA, physiotherapy can significantly improve quality of life and manage symptoms. Here’s how:
1. Pain Management:
Modalities like heat, cold therapy, or TENS (Transcutaneous Electrical Nerve Stimulation) can help reduce pain and inflammation, providing relief for those with OA. They can also give advice on exercise and activity modifications to make movements less painful.
2. Strengthening Exercises:
Strengthening the muscles surrounding the affected joint helps to stabilise and support the joint. This can reduce strain on the cartilage and decrease pain over time.
3. Range of Motion Exercises:
Physiotherapists can guide you through stretching and mobility exercises to maintain or improve the joint’s flexibility. This can help reduce stiffness and increase the range of motion.
4. Posture and Body Mechanics:
Physiotherapists can teach you how to adjust your posture and movement patterns to avoid putting additional strain on the affected joints, which can help in reducing pain and prevent further damage.
5. Weight Management:
If OA is in the weight-bearing joints (like the knees), physiotherapists may also work with you on strategies to reduce weight, as this can help reduce the load on the joints and alleviate symptoms.
6. Assistive Devices:
In some cases, a physiotherapist can recommend the use of assistive devices like braces, orthotics, or walking aids to support the affected joint and reduce pain during daily activities.
7. Education and Self-Management:
A physiotherapist can provide education on lifestyle modifications, including joint protection techniques, and ways to manage flare-ups of pain, allowing you to take control of your condition.
8. Aerobic Conditioning:
Gentle aerobic exercises (like walking, swimming, or cycling) can help improve cardiovascular health and overall stamina while avoiding high-impact stress on the joints.
In summary, physiotherapy focuses on reducing pain, improving movement, and preventing further deterioration, making it a key component of an overall management plan for osteoarthritis.
Here at Auckland Physiotherapy we are able to examine and diagnose your hip and knee condition and give you an individually tailored Arthritis care plan.
For more information, read about Arthritis Care at Auckland Physiotherapy or Mark Quinn's Blog on Arthritis Management. We also offer relief from arthritis packages.
For more information, come into our clinic (close to Remuera, Newmarket and Parnell) to speak to our expert team. It is essential you first get the right diagnosis before any treatment and management occur so book in for a first appointment.

Check out our Online Store for great Rehab and Health goods.


There are several common foot problems that people experience, and podiatry is a branch of medicine dedicated to diagnosing and treating these conditions. Here are some of the most common foot problems and how podiatry can help:
At Auckland Physiotherapy, our Podiatrist has been practising in musculoskeletal podiatry for 13 years and has studied for 9 years (so far…). He holds his Masters and is on track to finish his PhD in 2023. Meet Aaron Jackson here. To book an appointment, book online or call our team on 09 3664480.
Is that nagging neck pain affecting your daily life? You're not alone. Neck pain is one of the most common musculoskeletal conditions we treat. Let's explore effective strategies to manage and resolve your neck pain.
Understanding Neck Pain Common causes include:
Evidence-Based Treatment Approaches
Prevention Strategies Maintain good neck health by:
Recovery Timeline Most people experience improvement within:
Common Questions;
Mobilisations and massage can give you short term relief. For greater short- and long-term improvements in pain and quality of life, exercise combined with manual therapy give better results in comparison to manual therapy alone.
2. Do I need to see my GP before seeing a Physio?
No, you do not need to see your GP before seeing us at Auckland Physiotherapy. Our expert team can lodge your ACC claim and refer you for imaging and specialist reviews if required. Our Physiotherapists have a wealth of knowledge in assessing and diagnosing your pain. We believe this is the most important part of your recovery as once you know what is wrong, you can use the most evidenced based treatment specific for that condition.
3. Can Poor Posture cause neck pain?
Yes, absolutely. Poor posture, especially from sitting at a desk for long periods, looking down at a phone or hunching over can over time cause stress and strain to the muscles, ligaments and joints, leading to pain.
4. Is neck pain related to stress?
Yes, stress can cause muscle tension in the neck and shoulders, which can lead to pain and discomfort. It can also alter the way you breath which in turn makes you use your neck muscles to help you breath.
5. Can neck pain cause Headaches?
Yes, neck pain is often associated with tension headaches and migraines. The muscles around your neck and your upper neck joints can refer pain to your head. At Auckland Physio, we have a specialised Headache Clinic with our expert Masters Physio Robyn Atkinson, who works with people to overcome headaches. She uses the Evidenced-based Watson Approach.
6. Is neck pain common as we age?
Yes, neck pain tends to increase with age due to conditions like osteoarthritis or degenerative disc disease.
7. What can I do to prevent neck pain?
Regular exercise, maintaining good posture, good ergonomics and taking frequent breaks can help prevent neck pain. We suggest you see a Physiotherapist early to help instead of waiting.
For more information, come into our clinic (close to Remuera, Newmarket and Parnell) to speak to our expert team. It is essential you first get the right diagnosis before any treatment and management occur so book in for a first appointment.

Check out our Online Store for great Rehab and Health goods.


Frozen shoulder, or adhesive capsulitis, can be a frustrating and painful condition. This comprehensive guide will help you understand the condition and explore effective treatment options.
What is Frozen Shoulder? Frozen shoulder involves:
The Three Phases:
Treatment Approaches
Recovery Tips:
If you think you have a frozen shoulder, come to Auckland Physio, Parnell clinic to see one of our Physiotherapists. You can book easily online HERE or call our friendly reception team on 093664480. Alternatively, if you're not sure if Physio can help, book a Auckland Physio complimentary call.
Common Questions
Yes, Physiotherapy can be very effective in treating frozen shoulder (adhesive capsulitis). Physiotherapists use a combination of treatments to reduce pain, increase the range of motion, and improve function in the shoulder.
Common physiotherapy techniques at Auckland Physiotherapy include:
If you're dealing with frozen shoulder, it’s important to work closely with a physiotherapist who can guide you through exercises and treatments specific to your condition. It may take time, but physiotherapy can lead to significant improvement.
2. How long does it take for a Frozen Shoulder to go?
A frozen shoulder can be a slow and frustrating condition, and the recovery timeline can vary from person to person. Generally, it progresses through three stages:
1. Freezing stage (painful phase): This stage lasts 6 weeks to 9 months, where the shoulder becomes increasingly painful, especially with movement, and its range of motion starts to decrease.
2. Frozen stage (adhesive phase): This stage can last 4 to 6 months. The pain may decrease, but the shoulder becomes stiff, making it difficult to move. Function is limited.
3. Thawing stage (recovery phase): This can take anywhere from 6 months to 2 years. During this stage, the shoulder gradually regains mobility, and pain continues to decrease.
In total, recovery from a frozen shoulder can take anywhere from 1 to 3 years. Without treatment, spontaneous complete or nearly-complete recovery over a varied period of time occurs. However, with proper treatment, including physiotherapy, the recovery time can be shortened, and the condition can be managed more effectively. Regular stretching and strengthening exercises, along with professional guidance, can help speed up the recovery process and improve outcomes.
3. What causes frozen shoulder?
A Frozen Shoulder affects about 6% of the population. The exact cause is not fully understood, but it is often linked to shoulder injury, surgery, or conditions like diabetes, thyroid disorders, and heart disease. It can also occur without any apparent reason.
4. How do I know if I have a frozen shoulder?
Symptoms include pain and stiffness in the shoulder, difficulty moving the arm, especially in certain directions (like overhead or behind the back), a limited range of motion and pain sleeping on the affected side. At Auckland Physio, our expert Physio team will assess your shoulder and do a range of special tests to try and diagnose your pain. You may be asked to get an X-ray and Ultrasound to rule out any other injuries. You may also be referred to a specialist for further management.
5. Can frozen shoulder go away on its own?
Yes, but it can take a long time—sometimes up to 2 to 3 years. Treatment, like physiotherapy, can help speed up recovery and reduce pain.
6. Can physiotherapy cure frozen shoulder?
Physiotherapy can significantly help reduce pain, improve range of motion, and restore function, but full recovery can take time and may require a combination of treatments.
7. What are the risk factors for a Frozen Shoulder?
Common risk factors include age (typically 40-60 years old), diabetes, heart disease, recent shoulder surgery or injury, thyroid disorders, and prolonged immobility.
For more information, come into our clinic (close to Remuera, Newmarket and Parnell) to speak to our expert team. It is essential you first get the right diagnosis before any treatment and management occur so book in for a first appointment.

Check out our Online Store for Rehab and Health goods.


A Comprehensive Guide
Living with gluteal tendinopathy (also known as greater trochanteric pain syndrome) can be challenging, but effective treatment options are available. This condition affects the tendons that connect your gluteal muscles to your hip and can cause persistent pain on the outside of your hip.
In this condition, tendons are generally not inflamed, which is why traditional methods like rest and anti-inflammatory medications often don't resolve the issue. Most experts recognize the problem as being degenerative, which may sound intimidating, but it is something that can usually be treated successfully for most people.
To put it simply, the body experiences constant strain from physical activity, leading to wear, and then repairs itself during periods of rest. When the wear occurs faster than the body’s ability to repair, healthy tendons can become weakened and eventually painful.
Several factors influence this wear-and-repair process, such as the intensity of exercise, fitness level, body composition, hormonal shifts, stress, posture, limb alignment, and past injuries. Because of this, simply easing back into activity doesn’t always solve the problem, and a more tailored rehabilitation plan is often necessary. This rehab approach focuses on identifying the specific factors causing the issue and creating an exercise routine to strengthen the gluteal muscles and tendons, improving their ability to tolerate stress.
Tendons have a limited blood supply, meaning that healing and adapting to exercise is a slow process, which is why rehabilitation can take months. However, with consistency and patience, this method typically leads to long-term improvement and successful outcomes.
Key Treatment Approaches:
Prevention Tips:
If you need more information or need help with your hip pain, book a Physio session at Auckland Physiotherapy, Newmarket. If you are unsure who you would like to see, book a complimentary call and talk to one of our expert Physio's today.
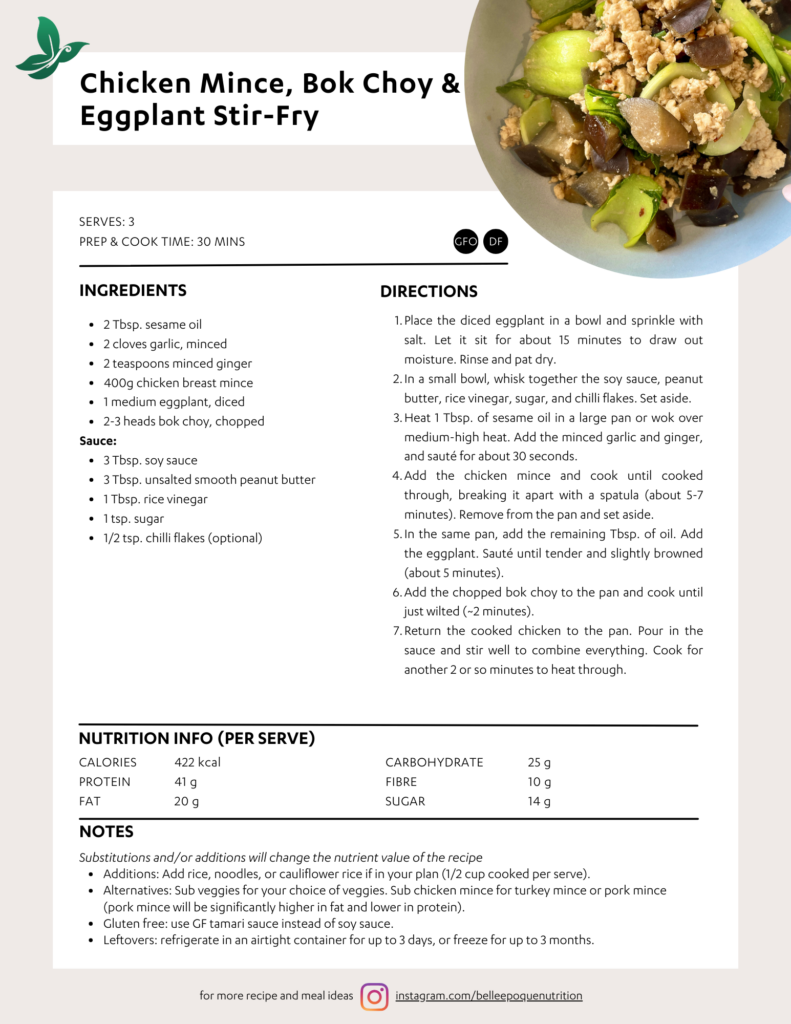
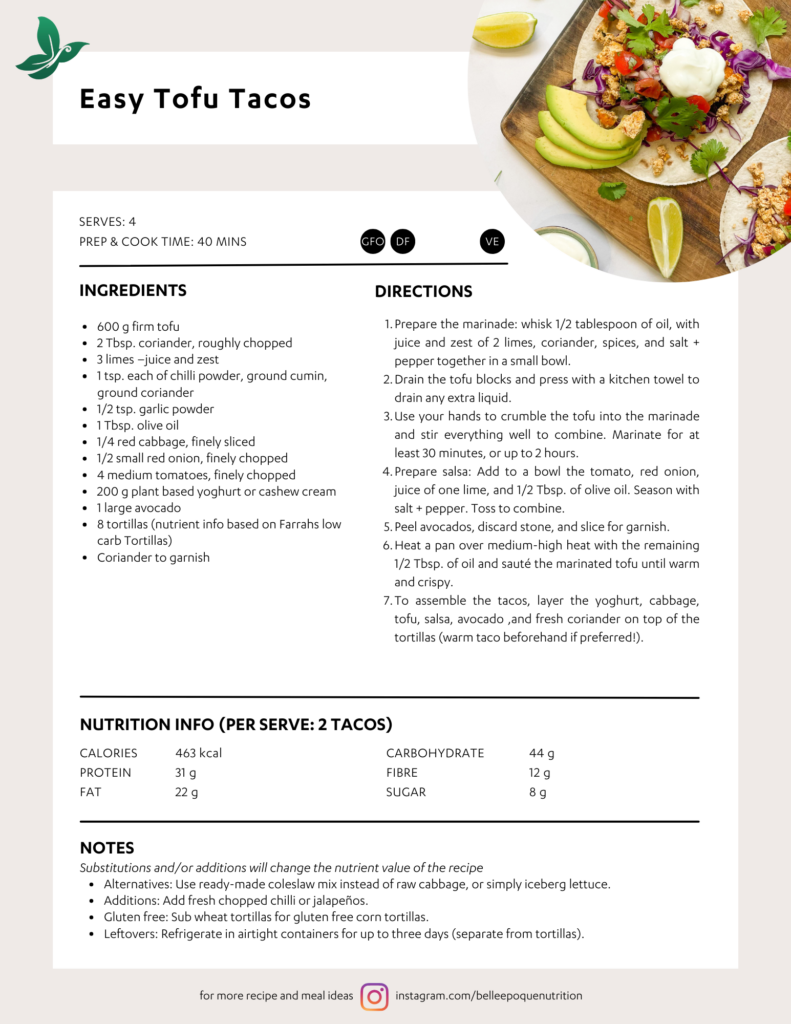
SERVES: 2
PREP & COOK TIME: 30 MINS
INGREDIENTS
SERVES: 2
PREP & COOK TIME: 30 MINS
250 g kumara, cut into 2 cm cubes
2 Tbsp. olive oil
280 g lean beef (e.g. sirloin), cut into 2 cm
strips, seasoned with salt and pepper
1/2 bag of leaves (e.g. rocket, baby spinach, or
mixed)
4 cherry tomatoes (or 1 medium tomatoes),
chopped
1/2 small red onion, diced
2 Tbsp. crushed peanuts, for garnish
Dressing:
2 Tbsp. low-sodium (salt) soy sauce
2 cloves garlic, crushed (OR 1 tsp. minced)
1 tsp. minced ginger
1/2 Tbsp. coconut sugar
1 Tbsp. rice wine vinegar
DIRECTIONS
Preheat oven to 200°C. Line an oven tray with baking
paper.
1. Toss kumara pieces with half the olive oil, and season
with salt and pepper. Roast for 25-30 minutes or until
golden and crispy.
2. To make the sauce, mix the soy, garlic, ginger, sugar,
and vinegar in a bowl. Set aside.
3. Heat the remaining olive oil in a pan over high heat.
Cook beef for about 2 minutes on each side (this is for
approx. med-rare, try more or less depending on your
preference).
4. In a large bowl, mix leaves with tomato, red onion and
kumara.
5. Divide salad between plates. Add beef strips and drizzle
everything with soy and ginger dressing. Garnish with
crushed peanuts.
NUTRITION INFO (PER SERVE)
CALORIES; 472 kcal
PROTEIN; 38 g
FAT; 18 g
CARBOHYDRATE; 38 g
FIBRE; 6 g
SUGAR; 12 g
NOTES
Substitutions and/or additions will change the nutrient value of the recipe
Additions: Add fresh herbs such as coriander, fresh chilli, other salad ingredients such as cucumber,
capsicum.
Alternatives: Sub beef for another protein of your choice, sub kumara for another root veg or pumpkin.
Gluten free: use GF tamari sauce instead of soy sauce. Ensure peanuts gluten free.
Leftovers: Refrigerate in an airtight container for up to 4 days. Keep salad separate from the kumara and beef so as to keep salad leaves fresh.
Sarah Mitchell Weston (PhD) is a Registered Nutritionist at belle époque nutrition in Grey Lynn. Sarah specialises in weight management, gut health, and sport nutrition, providing evidence based advice and personalised food plans. Appointments available in person or online, contact [email protected] for enquiries or to book.